Delayed surgeries. A mass staff exodus. A culture of fear. New IG reports outline issues at Colorado VA hospital

{image}{photoCredit}the associated press file{/photoCredit} {caption}Visitors stroll through a long, glass-walled corridor that connects a dozen buildings at the Rocky Mountain Regional VA Medical Center in Aurora after a ribbon-cutting ceremony at the hospital in 2018.{/caption} {standaloneHead}Colorado senators pressure VA to improve veteran health care (copy){/standaloneHead} {/image}
the associated press file
The Department of Veterans Affairs hospital in Aurora stopped all cardiac surgeries for 11 months amid an exodus of clinical staff and leadership problems that created a culture of fear.
That is according to two VA Office of Inspector General reports released last week. The documents outlined the problems that led to numerous clinical leaders departing the Rocky Mountain Regional VA Medical Center while regional leadership remained unaware or unengaged. In addition, the VA’s central offices were not notified that cardiac surgeries at the medical center were shut down, according to a report.
The leaders who left included the chief of hospital medicine, the chief of hematology and oncology, the chief of cardiothoracic surgery and the chief of anesthesiology, among others. All but one of the cardiac surgical staff resigned. The other employee was fired.
Residue found on medical equipment VA Hospital in Aurora still unidentified, cause remains unknown
A survey of former employees found a lack of trust and confidence in senior leaders and a fear of retaliation around reporting concerns. The report quoted former and current facility leaders anonymously about the problems. In some direct quotes, the employees complained specifically about the former facility director and former chief of staff.
“You are not encouraged to have opinions. And if your opinion differs, there are clear repercussions that can be anything from being berated in a meeting to being pushed out on the back end with some false accusations or claims that then have to be investigated, and people are removed from positions,” an employee told investigators about the former facility director, according to the report.
In October 2023, Network Director Sunaina Kumar-Giebel removed the director of VA Eastern Colorado Health Care, Michael Kilmer, and Shilpa A. Rungta, the chief of staff, from leadership. Two other leaders the reports cited as contributing to the negative culture resigned, according to a VA news release.
PERSPECTIVE: Serving Colorado’s vets
The recent report said investigators remain concerned about continued departures, low morale and “the potential current and future impact on patient safety and services.” The report did not find any patient harm in its reviews.
The current interim director of the facility who started in March, Amir Farooqi, addressed facility challenges in an interview Friday with The Gazette, covering the state of cardiac surgeries, morale, hiring, nurse concerns over staff shortages and the residue found on medical instruments that has affected nearly 500 surgeries and about 100 dental procedures.
While the hospital has the staff to complete cardiac surgeries, they are on pause along with all complex procedures because of the residue that has been identified as a kind of plastic. Farooqi could not say when the problem would be resolved, but a team is meeting every day to manage the patient care as a result of the hurdles. A team from the manufacturer of the sterilization equipment is coming next week to take the machines apart to identify the problem.
“It will literally be down to the screws,” Farooqi said.
In the meantime, the VA offers veterans the option to have surgeries scheduled at other community hospitals or wait for care. In clinical emergencies, the VA will send veterans to other hospitals, he said.
At the same time, unionized nurses rallied this week in front of the hospital over staffing shortages. In a news release, the union said 57 positions need to be filled to meet safe staffing standards.
The organization remains committed to working with the unionized nurses, Farooqi said.
“We are actively recruiting and hiring for nursing staff,” he said.
As for morale, Farooqi said the organization has been through challenging circumstances, but some employees have worked for the organization for decades and continue to be committed. Some have also offered constructive thoughts on improvements.
The VA said in a news release the new leadership has taken steps to correct problems identified in inspector general reports by holding monthly staff town halls and starting a project to revamp daily staff huddles, among other steps. The regional network that supervises the hospital also set up a new Office of Oversight.
Major change rocked ICU
The Office of Inspector General report found the VA paused heart surgeries for two weeks at the hospital in June 2022 because of a shortage of specialized nurse practitioners to care for patients 24/7. They restarted after the former chief of surgery and one other provider agreed to work night shifts in addition to their day shifts through September 2022, the report said.
In June 2022, the former cardiothoracic chief proposed hiring two specialized physician assistants to help provide care around the clock. The hiring didn’t take place.
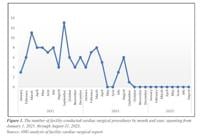
Without staff to provide constant care, the VA medical center did not provide any cardiac surgeries between October 2022 and August 2023. The medical center did not notify the VA’s central offices about the closure. The hospital used contract surgical staff to resume operations in late 2023, the report said.
During the pause, on Jan. 3, 2023, the chief of staff made the abrupt decision to stop allowing hospitalists to work in the ICU because of patient safety concerns. Hospitalists are similar to primary care doctors, but work strictly in hospitals.
The hospital planned to rely on specialists in the ICU instead, the report said, but it was “unsustainable” for them to provide 24/7 staffing.

Veterans Affairs Office of Inspector General
Veterans Affairs Office of Inspector General

Veterans Affairs Office of Inspector General
The day of the change, doctors completing their residency, or in-hospital training, were told that specialists would provide overnight on-call supervision while not at the hospital.
“After the change, ICU residents reported concerns to service leaders and in program evaluations citing lack of on-site supervision, increased patient safety risks, diminished resident education quality, and decreased overall satisfaction,” the report said.
In February 2023, the hospital told doctors completing residency to use a telehealth service for advice before calling an off-site supervisor but did not provide written guidance.
In March, the doctors in residency stopped using the telehealth service in their rounds during March, because it was unhelpful. The investigators did not find that the change in the ICU model resulted in harm after reviewing four cases.
Last week, the hospital brought on a new ICU medical director, Farooqi said. The hospital also now allows for hospitalists to provide overnight care in the ICU, he said.
Unsafe working conditions
Investigators found by surveying former facility leaders that a majority felt poor or unsafe working conditions contributed to their departures. The employees described the hospital as psychologically unsafe. A majority also said unethical treatment contributed to their departures, among other concerns.
Part of the problem was monopoly of control held by a handful of senior leaders, according to the inspector general reports.
“In a healthy leadership structure, a medicine chief would be able to advocate for the needs of patients and providers within the section,” a physician said in the report. “Instead, we do not have a safe and trusted supervisor, limiting checks and balances.”
The medical center is close to hiring a chief of hospital medicine and currently has someone acting in the role, Farooqi said.
During the exodus of staff, the reports found that senior leaders didn’t use exit surveys to identify why employees were leaving.
This year, Farooqi said the medical center really encouraged employees to share their thoughts and ideas through an all-employee survey and saw the highest response rate ever of around two-thirds of the staff participating. He said the data would be used to create action plans.
Rep. Jason Crow demands answers from VA over deleted prosthetic orders
The hospital could see greater oversight going forward because both reports called on the VA undersecretary for health, Dr. Shereef Elnahal, to provide more supervision of leaders at the regional level, an area that includes Colorado, Utah, Wyoming, Montana and portions of other states. The report calls on him to determine how regional leaders were unaware of the 11-month pause in surgeries and ensure regional leaders are involved in work at the Aurora center around clinical staffing and hiring and retention of employees, among other goals.
U.S. Rep. Jason Crow, D-Aurora, said in a recent statement he planned to continue to push for improvements to care at the medical center, an expansive facility that opened in 2018.
“I’m deeply concerned by the OIG’s report on pervasive staff culture issues and barriers to accessing medical care at the Rocky Mountain VA,” he said. “Veterans take an oath to serve and are promised quality care when they return home.”
Contact the writer at mary.shinn@gazette.com or 719-429-9264.